If you’ve been Googling wisdom teeth removal in Melbourne, you’re not alone. Wisdom teeth are the last molars to arrive, and they often make their entrance with a bit of drama. Some people get lucky and never notice them. Others deal with on-and-off symptoms for months, then suddenly end up with swelling and a frantic call for an urgent appointment.
Why wisdom teeth cause problems
Wisdom teeth can be blocked by bone, gum, or neighbouring teeth. When that happens, the tooth may only partly emerge or stay trapped, which makes the area harder to keep clean and more likely to inflame. That “trapped” position is common because many jaws simply don’t have enough room at the back.
Impacted wisdom teeth and what that really means
Dentists use the term “impacted” when a wisdom tooth can’t come through properly. It may sit at an angle, press into the tooth in front, or remain under the gum. X-rays help confirm the position and whether it’s harming nearby teeth.
The 4 signs your wisdom teeth need to go
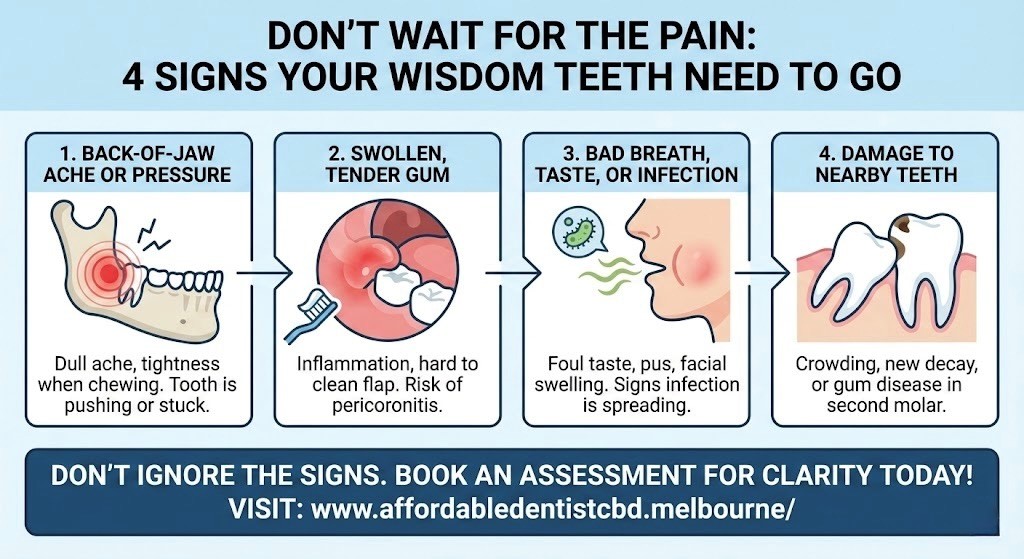
Below are four patterns dentists see again and again. You might notice one, or a messy mix of two or three.
| Sign | What you may notice | Why it matters |
| 1 | Back-of-jaw ache or pressure | The tooth is pushing or stuck |
| 2 | Swollen, tender gum behind the last molar | Inflammation around a partially erupted tooth |
| 3 | Bad breath/bad taste, ooze, swelling | Infection can spread if ignored |
| 4 | New decay or soreness near the second molar | Wisdom teeth can damage or trap food near the tooth in front |
Sign 1: A dull ache or pressure at the back of your jaw
This often feels like a tightness when you chew, or a sore spot that comes and goes. Some people also notice referred pain to the ear or temple. A tooth that’s struggling to erupt can irritate gum and jaw tissue even before a full-blown infection appears.
What to do: Book a check-up while the pain is still manageable. An exam and X-ray can show whether the tooth is angled into the tooth in front, or sitting in a position that’s likely to cause trouble later.
Sign 2: Swollen gum, bleeding, or a flap of gum you can’t keep clean
If you can see (or feel) a soft flap over the back tooth, food and plaque can get trapped underneath. That spot becomes tender, puffy, and sometimes bleeds when you brush. This type of inflammation around a partially erupted wisdom tooth is often linked with pericoronitis.
What to do: Keep the area as clean as you comfortably can and avoid poking at it. If swelling keeps returning, it’s usually a sign the tooth’s position is creating an ongoing hygiene problem rather than a one-off irritation.

Sign 3: Bad breath, bad taste, or swelling that suggests infection
Bad breath isn’t always about brushing technique. When gum tissue around a wisdom tooth becomes inflamed, bacteria and debris can collect in a pocket that’s difficult to reach. If things escalate, you may notice a foul taste, pus, facial swelling, fever, or trouble opening your mouth.
This is where delay can backfire. A wisdom tooth infection can move beyond a local gum problem, particularly if swelling spreads or you feel unwell. Victorian health guidance lists warning signs such as facial swelling, pus, difficulty opening the mouth or swallowing, and fever.
Seek urgent care if you have rapidly increasing swelling, fever, difficulty swallowing, or difficulty breathing.
Sign 4: Crowding, decay, or damage to the tooth in front
Sometimes the wisdom tooth itself isn’t the main casualty. The tooth in front (your second molar) can develop decay or gum disease because the area becomes a plaque trap. Wisdom teeth issues can also contribute to decay, gum disease, and even abscesses or cysts in some cases.
What to do: Don’t ignore a new cavity or tenderness at the very back of the mouth. If a wisdom tooth is the underlying cause, filling the damage without addressing the source can lead to repeat problems.
When to see a dentist vs an oral surgeon in Melbourne
Many people start with their general dentist, who can examine the area, take X-rays, and discuss whether monitoring is reasonable or removal is the safer option.
An oral surgeon may be recommended when the tooth is deeply impacted, close to nerves, angled awkwardly, or when sedation is preferred due to complexity or anxiety.
Risks such as dry socket, infection, and injury to nearby structures are part of the standard discussion for extractions, particularly with more difficult impactions.
What wisdom tooth removal typically involves
- Most extractions begin with an assessment and imaging.
- The procedure itself may use local anaesthetic, sedation, or (less commonly) general anaesthetic depending on the case and setting.
- After removal, the socket forms a clot and heals over time.
- If that clot is lost too early, it can lead to a painful complication called dry socket, with severe pain and an “empty” looking socket.
Cost and appointment planning in Melbourne
Fees vary widely depending on how many teeth are removed, whether the teeth are impacted, and what type of anaesthetic is used. The most reliable way to get clarity is an examination and X-ray, followed by a written treatment plan.
If you’re looking for an assessment in the CBD, schedule a consultation with Affordable Dentist CBD through the website.
Also Read: A Definitive Guide to Wisdom Tooth Extraction Preparation
Frequently Asked Questions:
- How do I know if my wisdom teeth need to be removed?
A dentist considers symptoms, X-rays, and whether the tooth is likely to cause repeat infections, damage nearby teeth, or remain impossible to clean. - Should I remove wisdom teeth before they hurt?
Sometimes, yes. Teeth that are angled, partly erupted, or damaging the tooth in front can cause problems even when pain is mild. Monitoring can be reasonable when there are no signs of disease. - When is wisdom tooth pain an emergency?
Seek urgent care for facial swelling, fever, pus, trouble opening the mouth, difficulty swallowing, or any breathing difficulty. - How long does it take to recover?
Most swelling and soreness settles over several days, but full healing takes longer. Your clinician will give advice based on the complexity of your extraction. - What can I eat after wisdom teeth removal?
Soft foods are usually easiest at first. Avoid anything that irritates the wound or dislodges the clot, and follow the specific instructions you’re given.
If you’re noticing recurring swelling, bad taste, or persistent soreness at the back of your jaw, a straightforward check-up can prevent a small problem turning into a painful week.



