Third molars, commonly called wisdom teeth, can sit quietly for years or stir up trouble with little warning. Whether they emerge fully, stay buried, or only partly break through the gum, the approach to care shifts with age, anatomy and symptoms. Here’s a clear guide to what to expect across life stages, and when wisdom teeth removal in Melbourne makes sense.
Why wisdom teeth are removed (and when they’re not)
Dentists don’t remove third molars on a whim. They look for signs such as impaction, repeated gum infection (pericoronitis), decay that’s hard to treat, cysts, or damage to nearby teeth. Teeth.org.au highlights these issues as common reasons to extract, while also noting that symptom-free, disease-free teeth don’t automatically need surgery.
Another study reports that when surgery is performed at older ages, people experience higher rates of post-operative pain and complications. This doesn’t mean “the earlier the better” for everyone. It means decisions weigh current disease, future risk, and surgical difficulty, including root formation and bone density that increase with age.
1. Teens (15–19): monitoring first, timely action when needed
During the later teen years, roots are still forming and jawbone is more forgiving, which can make surgery simpler when extraction is indicated. For many teens, regular checks and X-rays track eruption and space. Removal is considered when there’s impaction with recurrent pericoronitis, deep decay that can’t be restored, or early signs of damage to the second molar.
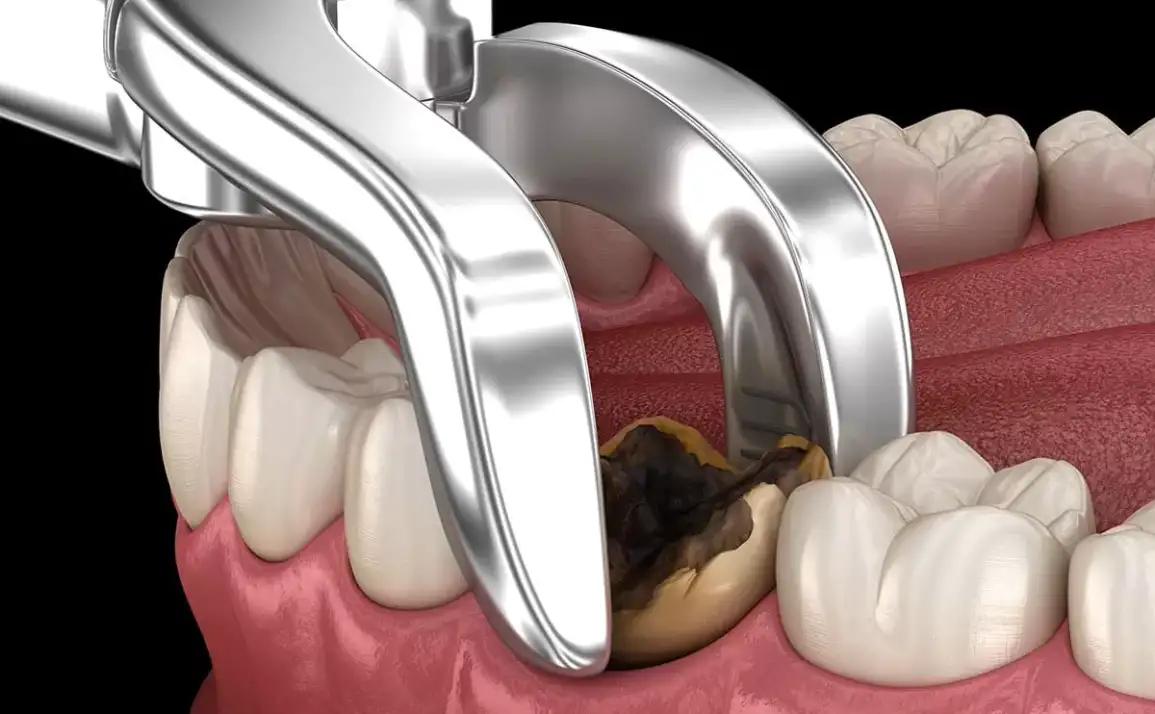
What the procedure involves: most upper third molars are relatively straightforward under local anaesthetic; lower ones tend to be trickier because of thicker bone and nearby nerves. Your dentist or oral surgeon will outline whether a simple lift or a surgical approach (lifting the gum, removing a small amount of bone, and sectioning the tooth) is expected.
Recovery in this age group is usually brisk. Swelling peaks around day two to three, then settles; pain is typically managed with a short course of analgesics and careful aftercare.
2. Early 20s (20–24): the “decision window”
Many symptomatic third molars declare themselves in the early 20s. Pericoronitis around a partly erupted lower tooth is a common story in general practice. Antibiotics alone won’t fix the underlying problem if gum flaps keep trapping debris. If infections repeat or hygiene access remains poor, extraction is usually recommended.
For those with symptom-free, impacted teeth, watchful waiting remains reasonable, with periodic review to catch decay on the back of the second molar or early gum disease.

3. Late 20s to 30s: balancing risk and benefit
By the late 20s and 30s, roots are fully formed and bone is denser, which can lengthen surgery and recovery. If disease is present (such as decay that can’t be restored, cyst formation, or periodontal pockets behind the second molar) removal still offers clear benefit. Expect your clinician to discuss nerve proximity, surgical complexity, and anaesthesia options in more detail at this stage.
Complication risk edges up with age, so meticulous planning matters. Experts note increased discomfort and postoperative issues in older cohorts, underscoring the value of timely treatment once pathology is confirmed.
4. 40s and beyond: targeted interventions
From mid-life onwards, third molars that never caused grief are less likely to erupt further. When problems do arise, such as caries creeping under the gum margin, fracture, or cysts, the calculus shifts to targeted surgery with careful risk counselling. Recovery can take longer, and clinicians pay extra attention to systemic health and medications.

Recovery: what normal looks like
A typical course involves oozing on day one, swelling peaking at 48–72 hours, and steady improvement from day four. Cold packs in the first 24 hours, head elevation, and prescribed pain relief help. Stick to soft foods at first and keep the wound clean with gentle saltwater rinses after the initial day. Your clinician will give specific instructions.
Dry socket (alveolar osteitis) is an uncommon but painful hiccup when the blood clot dislodges. Avoid smoking and vigorous rinsing early on, skip straws, and follow your dentist’s hygiene plan to lower the risk. Seek review promptly if pain escalates after initially improving.
Also Read: A Definitive Guide to Wisdom Tooth Extraction Preparation
Signals you shouldn’t ignore
Book a dental review if you notice repeated swelling near a partly erupted tooth, bad taste or discharge, decay on the back of the second molar, or jaw stiffness tied to the area. These patterns often point to pericoronitis or hard-to-clean pockets that keep flaring.
The bottom line
Across ages, the best approach to wisdom teeth in Melbourne is case-by-case. Teeth with disease, repeated infections, or risk to neighbouring teeth are candidates for removal. Symptom-free, disease-free teeth can often be observed with periodic review. Earlier treatment, when clearly indicated, tends to be simpler and better tolerated, and sound aftercare smooths recovery at any age.